The name of the condition that creates the pain that plagues so many! You’d be hard-pressed to find a human being that has not experienced pain and inflammation in their joints.
For some, the path was simple abuse and/or over-use without adequate care/time allowed for healing and repair. For others, it was a more metabolically mediated process where they were either chronically dehydrated or mineral imbalanced, or for many it happened through the process of consuming foods that triggered subclinical (sterile) inflammation.
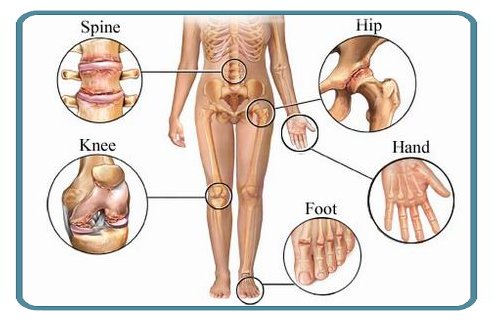
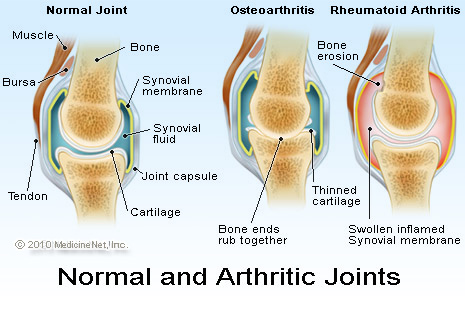
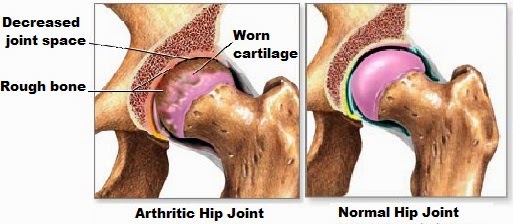
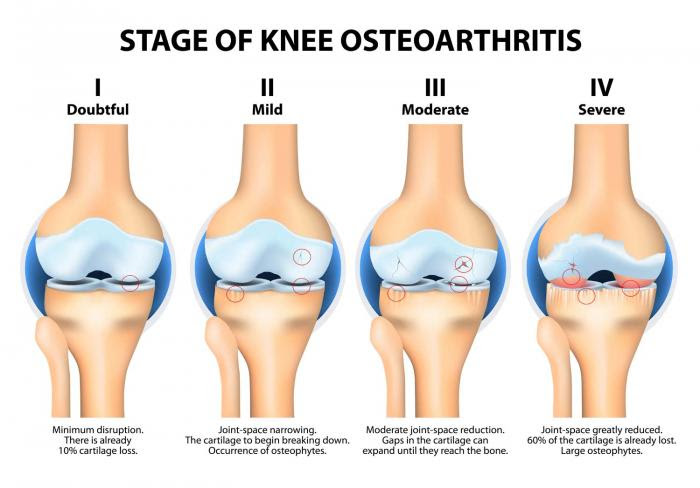
Regardless of the initiating event, this process involves the development of excessive tension within an area of the joint cartilage. This biomechanical stress produces structural and biochemical changes within the cartilage, which result in the formation of pro-inflammatory chemical reactions. This leads to the destruction of cartilage and joint fluid. As cartilage and joint fluid break down, the joint loses its ability to absorb shock and more stress is applied to the adjacent bone. The surrounding bone degenerates and over-proliferates, forming spurs.
All of these metabolic and structural pathways cause a common state of inflammation that muscles respond to unfavorably and chronic muscle tension results. This leads to a reduction in the normal range of motion and the joints fail to hydrate adequately through regular daily movement. This reduction in motion results in joint inflammation and varying degrees of degeneration which we call osteoarthritis.
Interestingly, when the food sensitivity mediated inflammatory process is allowed to continue unabated there is a strong probability of the arthritic process to turn into an autoimmune driven process. The Autoimmune inflammatory process of joint inflammation includes Rheumatoid Arthritis (RA), and Juvenile Rheumatoid Arthritis (JRA). In the Functional Medicine realm, we address these conditions by targeting inflammatory processes at their core in a uniform fashion.
This process starts in the gut.
Over half of the body’s immune system is localized around the gastrointestinal tract. This means that anything that over–activates the intestinal immune system can result in a contribution to the arthritic process via cytokine formation. Some of the things that can activate the intestinal immune system include parasites, bacteria, viruses, fungi, toxins, and food antigens. A food antigen is a particle of food that is recognized by the immune system as a foreign invader. Although an individual can react to any food, some of the most common food triggers are wheat, dairy, citrus, yeast, nightshades, histamines, and shellfish.
Getting the repair process going functionally requires first stopping the inflammation and secondarily reading the environment where the joint can repair.
Joint repair is influenced by numerous factors, including pH balance. Synthesis of new connective tissue is markedly impaired by excess tissue acidity. Acids are formed in response to consuming excess animal protein, grains, sugar, coffee, and alcohol. Stress, toxicity, and deficiencies of many nutrients also increase body acid. Aerobic exercise, hydration, and consumption of vegetables help neutralize acid.
Several other supplements are often helpful in cases of osteoarthritis. Niacinamide is one of these. High and frequent doses of niacinamide have been found to be very effective. Niacinamide can ease pain and stiffness, resulting in measurable increases in a joint’s range of motion as long as supplementation is continued and particularly so when inflammatory triggers are avoided.
There is so much that can be done for arthritic pain and even for the actual joint degeneration. The Functional Medicine model provides solutions for patients regardless of the pathways that brought them to their state of inflammation. The patient just needs to be willing to take an active role in their care beyond swallowing a pill to mask their pain.